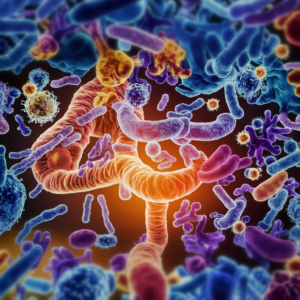
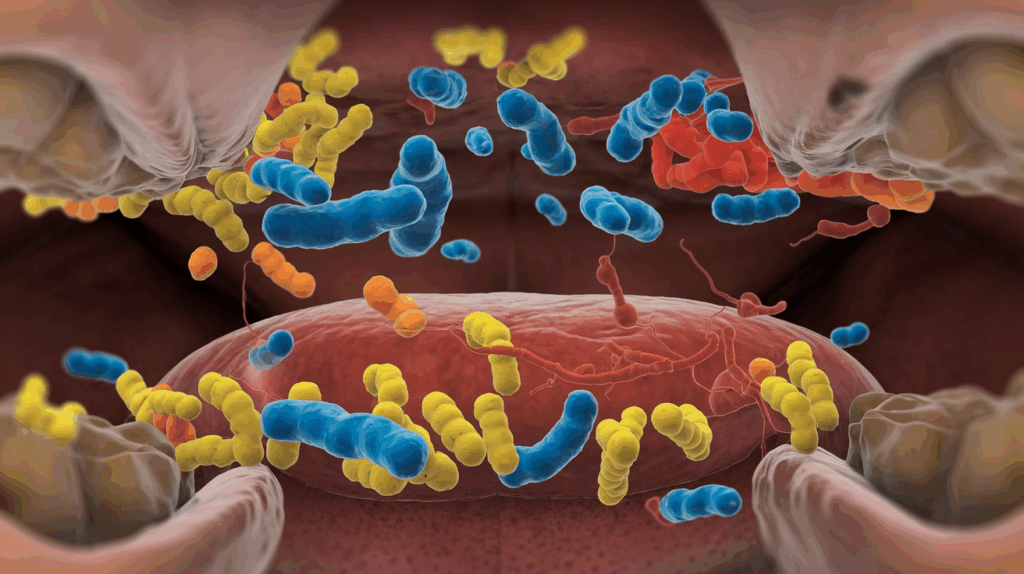
The human mouth is home to a complex ecosystem of over 700 species of microorganisms, collectively known as the oral microbiome. This intricate community plays a role not only in maintaining oral health but also in influencing systemic health and inflammation.
Understanding the Oral Microbiome
From birth, our oral cavity becomes colonised by a diverse array of bacteria, fungi, viruses, and protozoa. This microbiome aids in the initial stages of digestion, protects against pathogenic invasions, and contributes to the maintenance of oral tissues. Factors such as diet, oral hygiene practices, medications, and lifestyle choices continually shape its composition. A harmonious balance within this microbial community is essential.
Distruptions, known as dysbiosis, can lead to oral diseases like dental caries and periodontitis. More intriguingly, emerging research indicates that oral dysbiosis may have far-reaching effects beyond the mouth, impacting systemic health.
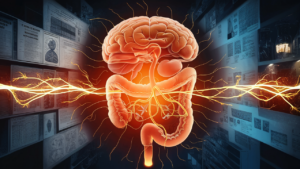
The Inflammation Connection
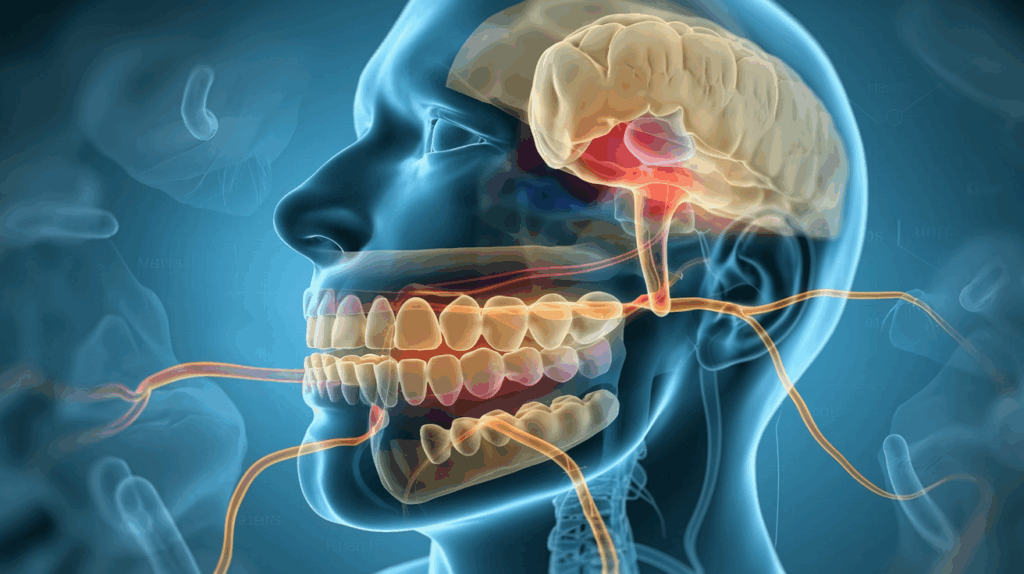
At the heart of the oral microbiome’s influence on systemic health is inflammation. When harmful bacteria overgrow in the mouth, they trigger an immune response, causing inflammation of the gums (gingivitis) that can progress to periodontitis, a more serious condition affecting the tissues and bone supporting the teeth. The inflamed, bleeding gums characteristic of periodontal disease create an entry point for oral bacteria to enter the bloodstream. Once in circulation, these bacteria and their byproducts can trigger inflammatory responses throughout the body, potentially contributing to or exacerbating various health conditions.
Beyond the Mouth: Conditions Linked to Oral Health
The research connecting oral health to systemic conditions grows more compelling each year. Here are some of the most significant associations:
Cardiovascular Disease
The link between oral health and heart disease is one of the most well-established connections. People with periodontal disease have a higher risk of experiencing cardiovascular events such as heart attacks and strokes. Several mechanisms explain this relationship:
- Oral bacteria like Porphyromonas gingivalis have been found in atherosclerotic plaques.
- Inflammatory markers triggered by oral bacteria contribute to arterial inflammation.
- The body’s immune response to oral pathogens may increase blood clotting factors.
Diabetes
The relationship between diabetes and oral health works both ways:
- People with diabetes are more susceptible to periodontal disease due to compromised immunity and blood vessel changes.
- Conversely, periodontal inflammation makes glycemic control more difficult, creating a vicious cycle.
- Treatment of periodontal disease has been shown to improve glycaemic control in some diabetic patients.
Rheumatoid Arthritis
The similarities between periodontal disease and rheumatoid arthritis (RA) are strong:
- Both involve chronic inflammation and bone destruction.
- P. gingivalis can modify proteins in a way that may trigger autoimmune responses associated with RA.
- RA patients with periodontal disease often see improvement in arthritis symptoms when their oral health improves.
Alzheimer’s Disease and Cognitive Decline
The emerging connection between oral health and neurodegenerative diseases has garnered significant attention:
- Oral bacteria have been found in the brains of Alzheimer’s patients.
- P. gingivalis produces enzymes called gingipains that have been linked to neuronal damage.
- Chronic inflammation from periodontal disease may contribute to inflammatory processes in the brain.
Respiratory Infections
The proximity of the mouth to the respiratory tract creates a natural pathway for oral bacteria to affect lung health:
- Aspiration of oral pathogens can contribute to pneumonia, especially in vulnerable populations.
- Periodontal disease has been associated with increased risk and severity of chronic obstructive pulmonary disease (COPD).
Pregnancy Complications
The oral-systemic connection extends to pregnancy outcomes:
- Periodontal disease has been associated with preterm birth and low birth weight.
- Maternal oral bacteria can be transmitted to the fetus, potentially affecting the development of the infant’s microbiome.
The Biological Mechanisms
How exactly does the oral microbiome influence these distant systems?
Several pathways have been identified:
Direct Invasion
Some oral bacteria possess the ability to enter the bloodstream and colonise distant sites. For example, oral streptococci can attach to damaged heart valves, causing infective endocarditis.
Inflammatory Mediators
Periodontal disease increases levels of pro-inflammatory cytokines like IL-1, IL-6, and TNF-alpha, which circulate throughout the body and can promote inflammation in various tissues.
Molecular Mimicry
Certain oral bacteria produce proteins that resemble human proteins, potentially triggering autoimmune responses where the body attacks its own tissues.
Microbial Metabolites
Byproducts of oral bacteria can enter circulation and affect distant organs. For instance, lipopolysaccharides (LPS) from gram-negative bacteria can trigger inflammatory responses in the liver and blood vessels.

Nurturing a Healthy Oral Microbiome
Given these connections, maintaining oral microbial balance becomes not just a matter of preventing cavities, but a significant strategy for overall health.
Balanced Oral Hygiene
The goal is not to eliminate all bacteria but to maintain a harmonious microbial environment:
- Brushing and Flossing: Brush thoroughly but gently twice daily and floss daily to remove bacteria from between teeth.
- Mouthwash Use: Be cautious with antiseptic mouthwashes; daily use can disrupt beneficial bacteria. Opt for natural rinses like saltwater or baking soda solutions.

Nutrition for Oral Health
Diet significantly influences the oral microbiome:
- Limit Sugars: Reduce intake of refined sugars and processed carbohydrates that feed harmful bacteria.
- Consume Prebiotics: Foods like garlic, onions, and asparagus support beneficial bacteria.
- Vitamins and Minerals: Ensure adequate intake of vitamin C for gum health and vitamin D, which has antimicrobial properties and reduces inflammation.
Lifestyle Factors
Several habits impact oral microbial health:
- Avoid Smoking: Tobacco use severely disrupts oral microbial balance.
- Manage Stress: Chronic stress can reduce immune function and alter the microbiome.
- Stay Hydrated: Saliva contains antimicrobial compounds and helps maintain balance.
- Adequate Sleep: Proper rest supports immune function and microbial homeostasis.
Professional Care
Regular dental visits are important:
- Professional Cleanings: Remove biofilm that cannot be eliminated at home.
- Early Intervention: Prevent progression from gingivitis to periodontitis.
- Comprehensive Evaluation: Dentists can identify signs of systemic conditions that manifest in the mouth.
The Future of Oral-Systemic Health
Research into the oral microbiome is advancing rapidly, with promising developments on the horizon:
- Salivary Diagnostics: Using saliva samples to detect biomarkers for various diseases.
- Targeted Probiotics: Developing oral probiotics that specifically combat pathogenic bacteria.
- Personalised Oral Care: Tailoring recommendations based on individual microbiome analysis.
- Integrated Healthcare Models: Bringing dental and medical professionals together to address oral-systemic connections.
Conclusion
The understanding of the oral microbiome makes us reconsider the separation between oral health and overall health. Your mouth is not just a gateway to your digestive system, it is a complex ecosystem intimately connected to your entire body through multiple biological pathways.
As research continues to elucidate these connections, one thing becomes increasingly clear: caring for your oral microbiome is not just about preventing cavities or maintaining a bright smile. It is a fundamental component of a holistic approach to health that recognises the interconnectedness of all body systems.
The next time you reach for your toothbrush, remember: you are not just cleaning your teeth. You are nurturing an ecosystem that influences your entire body’s well-being.
References
Golijanin, J., Kozić, J., Milinković Knežević, S., & Todorović, L. (2022). The Oral Microbiome and Systemic Diseases: A Two-Way Street. Biomedicines, 10(11), 2834.
Niu, Y. (2022). Editorial: The Pivotal Role of Oral Microbiota Dysbiosis and Microbiota-Host Interactions in Diseases. Frontiers in Cellular and Infection Microbiology, 12, 9267765.
This article is for informational purposes only and does not constitute medical advice. Always consult with qualified healthcare professionals regarding any health concerns.