Table of Contents
Introduction
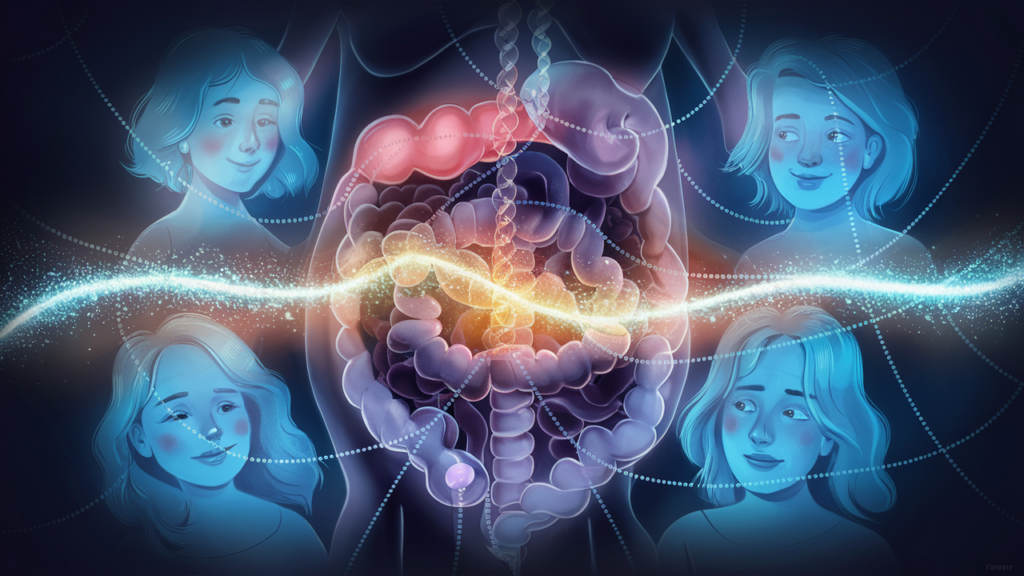
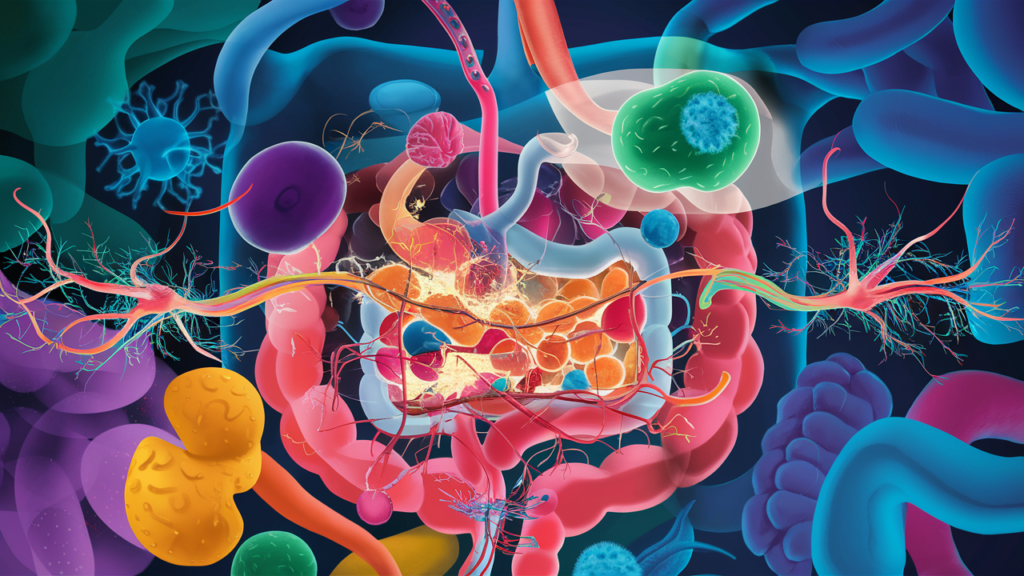
The gut-brain axis has received a lot of attention in recent years as researchers uncover the complex connections between gut health and brain function. This two-way communication not only affects digestion but also has an impact on mental well-being, neurological disorders, and overall health. It is important to understand the gut-brain axis to develop effective strategies for promoting overall well-being and preventing or managing various health conditions.
What is the Gut-Brain Axis?
The gut-brain axis refers to the complex communication network that connects the central nervous system (CNS) – primarily the brain and spinal cord – with the enteric nervous system (ENS), which governs the function of the gastrointestinal tract. This axis ensures that the brain can influence gut functions and vice versa.
It involves various components, including the vagus nerve, enteric nervous system, immune system, endocrine system, gut microbiome, hypothalamus, and pituitary axis.
The Gut-Brain Communication Pathways
The gut and brain are intricately connected through a complex network of bidirectional communication pathways, facilitating a constant exchange of signals and information. These pathways allow the gut microbiome to influence brain function and behaviour, while the brain, in turn, can modulate gut activity and the composition of the gut microbiome. Understanding these communication pathways is crucial to unravelling the intricate gut-brain connection.
Key components of the gut-brain axis include:
1. Vagus Nerve: The vagus nerve is a major pathway that connects the brain and the gut. It carries bidirectional signals, allowing communication between the two. Through the vagus nerve, the brain can influence gut function and vice versa. It plays a role in regulating digestion, inflammation, and even mood. Neurotransmitters like serotonin, dopamine, and acetylcholine are involved in the communication along the vagus nerve.
2. Enteric Nervous System: The enteric nervous system is a complex network of neurons within the walls of the gastrointestinal tract. It can operate independently and communicates with the brain via the vagus nerve. The enteric nervous system regulates various gut functions, including digestion, absorption, and motility. It also produces neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA) that modulate gut and brain function.
3. Immune System: The immune system plays a vital role in the gut-brain axis. Inflammatory molecules released by immune cells in the gut can communicate with the brain and impact mood and behaviour. Cytokines, such as interleukin-6 (IL-6) and tumour necrosis factor-alpha (TNF-alpha), are involved in these immune responses and can influence brain function.
Cytokines are small proteins released by immune cells that have a specific effect on cell communication and behaviour. They are crucial in the gut-brain axis, as they can influence both gut and brain functions.
Pro-inflammatory Cytokines:These include interleukin-6 (IL-6) and tumour necrosis factor-alpha (TNF-α). Elevated levels of pro-inflammatory cytokines are associated with various diseases and can affect brain function, contributing to mood disorders and neurodegenerative diseases.
Anti-inflammatory Cytokines: Examples include interleukin-10 (IL-10). These cytokines help to reduce inflammation and maintain homeostasis in the gut-brain axis.
4. Endocrine System: Hormones produced by the endocrine system can also influence the gut-brain axis.
Cortisol: Known as the stress hormone, is released by the adrenal glands in response to stress. Chronic stress and elevated cortisol levels can negatively impact gut health, leading to conditions like irritable bowel syndrome (IBS).
Serotonin: Approximately 90% of the body’s serotonin, a neurotransmitter that regulates mood, is produced in the gut. Serotonin influences gut motility and function, and imbalances can contribute to mood disorders such as depression and anxiety.
Ghrelin: This hormone, produced in the stomach, stimulates appetite and plays a role in energy balance. Ghrelin also affects mood and cognitive functions.
Leptin: Produced by adipose tissue, regulates energy balance and suppresses appetite. Leptin resistance is linked to obesity and metabolic disorders, which can affect brain health.
These gut-derived hormones can cross the blood-brain barrier and interact with receptors in the brain, modulating various physiological processes, including appetite, mood, and cognitive function.
5. Gut Microbiome: The gut microbiome refers to the trillions of microorganisms, including bacteria, archaea, viruses, and fungi, residing in the gastrointestinal tract. These microorganisms produce various metabolites, neurotransmitters, and molecules that can influence both gut function and brain health. For example, certain bacteria can produce neurotransmitters like serotonin and dopamine, as well as short-chain fatty acids (SCFAs) like butyrate, which can modulate brain function.
Diversity and Function of the Gut Microbiome
Digesting Food: Microbes help break down complex carbohydrates and fibres that the human body cannot digest on its own.
Synthesising Vitamins: Certain gut bacteria produce essential vitamins, such as B vitamins and vitamin K.
Regulating Immune Function: The gut microbiome influences the development and function of the immune system, promoting a balanced immune response.
Protecting Against Pathogens: Beneficial microbes compete with harmful pathogens for nutrients and attachment sites, inhibiting their growth.
The Gut-Brain Connection
The gut microbiome communicates with the brain through multiple pathways:
– Neural Pathways: The vagus nerve is a primary conduit for signals between the gut and the brain.
– Immune Pathways: The gut microbiome modulates the immune system, influencing inflammation and cytokine production.
– Endocrine Pathways: Gut microbes can produce and modulate hormones and neurotransmitters that affect brain function.
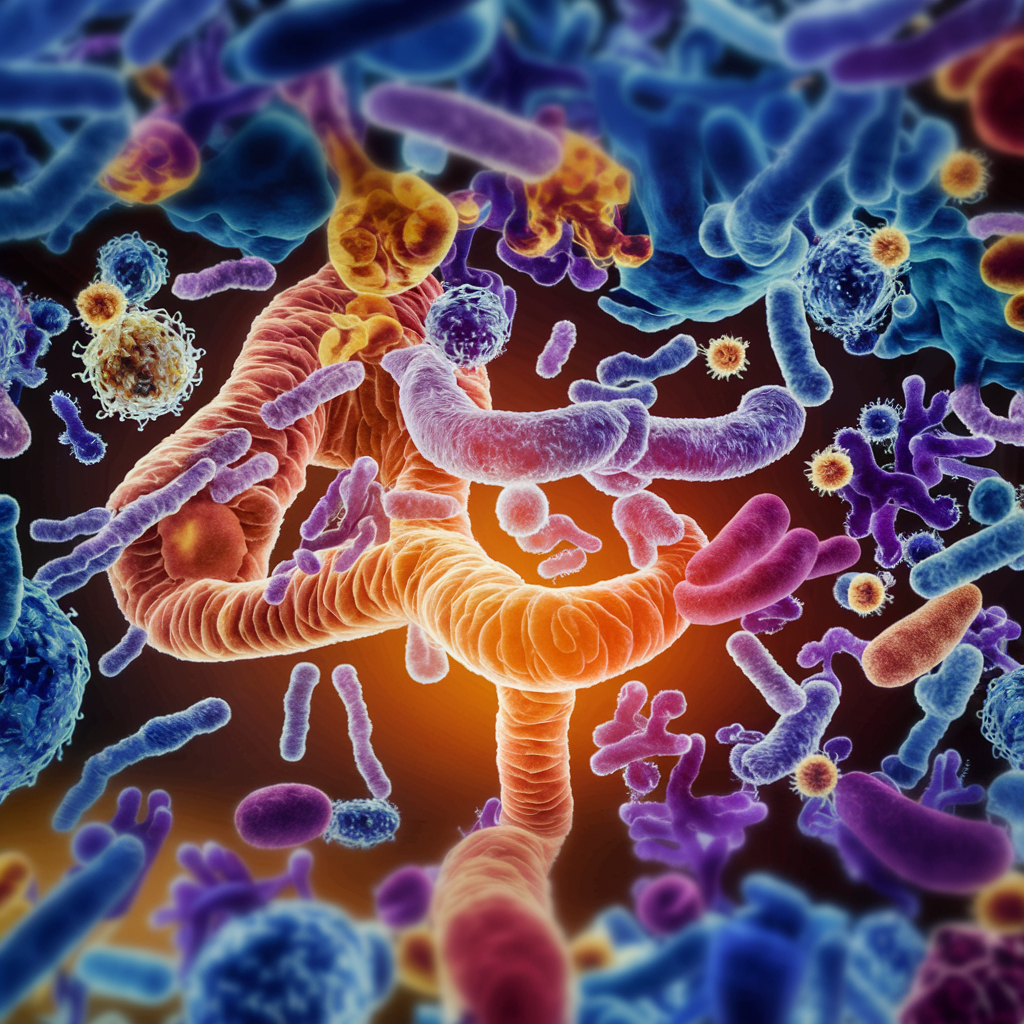
Dysbiosis and Its Impacts
Dysbiosis refers to an imbalance in the gut microbiome, where harmful microbes outnumber beneficial ones. This imbalance can result from factors such as poor diet, antibiotics, chronic stress, and illness. Dysbiosis is linked to various health issues, including:
– Gastrointestinal Disorders: Conditions like IBS and inflammatory bowel disease (IBD) are associated with dysbiosis.
– Mental Health Disorders and Neurodegenerative Diseases: Dysbiosis has been implicated in mood disorders, such as depression and anxiety, and neurodegenerative diseases through its impact on inflammation and neurotransmitter production.
– Metabolic Disorders: An imbalanced gut microbiome can contribute to obesity, diabetes, and metabolic syndrome.
The Gut-Brain Barrier
The gut-brain barrier is a selective barrier that regulates the passage of molecules from the gut into the bloodstream and, ultimately, the brain. This barrier is formed by specialised cells called enterocytes, which are tightly joined together by protein complexes called tight junctions.
A healthy gut-brain barrier maintains a delicate balance, allowing the passage of essential nutrients while preventing harmful substances from entering the bloodstream. However, certain factors, such as chronic stress, inflammation, and an imbalanced gut microbiome, can increase the permeability of this barrier, leading to a condition known as “leaky gut.”
In a leaky gut scenario, bacterial metabolites, toxins, and other substances that would normally be contained within the gut can enter the bloodstream and potentially reach the brain. This can trigger an inflammatory response and contribute to the development or exacerbation of various neurological and psychiatric conditions.
Furthermore, increased gut permeability has been associated with the passage of larger molecules, such as lipopolysaccharides (LPS) from gram-negative bacteria, which can activate the immune system and contribute to neuroinflammation and neurodegeneration.
6. Hypothalamus and Pituitary Axis: The hypothalamus and pituitary gland are key components of the brain that play a crucial role in regulating various physiological processes, including stress response, hormone secretion, and autonomic functions. The hypothalamus regulates the release of hormones from the pituitary gland, which, in turn, controls the release of hormones from other endocrine glands. These hormones, such as adrenocorticotropic hormone (ACTH) and growth hormone, can influence both the gut and the brain.
Components of the HPA Axis
1. Hypothalamus: The hypothalamus is a small region at the base of the brain that plays a crucial role in hormone production and regulation. It releases corticotropin-releasing hormone (CRH) in response to stress.
2. Pituitary Gland: Upon receiving CRH signals from the hypothalamus, the pituitary gland secretes adrenocorticotropic hormone (ACTH) into the bloodstream.
3. Adrenal Glands: ACTH stimulates the adrenal glands, located on top of the kidneys, to produce and release cortisol, the primary stress hormone.
The Role of the HPA Axis in the Gut-Brain Communication
The HPA axis is integral to the stress response and influences both the brain and the gut. Chronic activation of the HPA axis due to prolonged stress can have several adverse effects:
– Gut Health: Elevated cortisol levels can increase gut permeability (often referred to as “leaky gut”), disrupt the balance of gut microbiota, and lead to gastrointestinal issues such as IBS.
– Brain Health: Persistent high cortisol levels can impair cognitive functions and contribute to mood disorders like depression and anxiety.
The interplay between these components and molecules is complex, and disruptions or imbalances within the gut-brain axis can influence mental health and well-being. Understanding the intricate connections and communication pathways within the gut-brain axis is an active area of research, and further exploration is needed to fully comprehend its complexities and potential therapeutic interventions.
Diet and the Gut-Brain Axis
Diet plays a crucial role in shaping the gut microbiome and, by extension, the gut-brain axis. Different dietary components can either support a healthy microbiome or contribute to dysbiosis.
– Fibre: Dietary fibre, found in fruits, vegetables, whole grains, and legumes, is essential for a healthy gut microbiome. Fibre is fermented by gut bacteria, producing short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory and neuroprotective effects.
– Probiotics and Prebiotics: Probiotics are live beneficial bacteria found in fermented foods like yoghurt, kefir, sauerkraut, and kimchi. Prebiotics are non-digestible fibres that feed these beneficial bacteria. Consuming both can support a healthy gut microbiome.
– Polyphenols: These plant compounds, found in foods like berries, tea, and dark chocolate, have antioxidant and anti-inflammatory properties that benefit gut health.
– High-Fat and High-Sugar Diets: Diets high in saturated fats and sugars can promote dysbiosis and inflammation, negatively impacting both gut and brain health.
– Mediterranean Diet: Rich in fruits, vegetables, whole grains, nuts, and olive oil. The Mediterranean diet is associated with a lower risk of depression and cognitive decline.
– Western Diet: Characterised by high intake of processed foods, sugars, and unhealthy fats. The Western diet is linked to increased inflammation and a higher risk of mental health disorders such as depression and anxiety.
Mechanisms Behind Diet’s Impact on the Gut-Brain Axis
1. Microbiota Composition: Diet directly influences the composition and diversity of the gut microbiota. A diverse microbiota is associated with better health outcomes, whereas a less diverse microbiota can lead to dysbiosis and associated diseases.
2. Metabolites Production: Gut bacteria produce metabolites that can affect brain function. For example, SCFAs produced from fibre fermentation have anti-inflammatory and neuroprotective properties.
3. Inflammation Modulation: Diet influences systemic inflammation. Anti-inflammatory diets (rich in fibre, polyphenols, and omega-3 fatty acids) can reduce inflammation, while pro-inflammatory diets (high in refined sugars and saturated fats) can exacerbate it.
4. Neurotransmitter Synthesis: Certain nutrients and gut bacteria are involved in the synthesis of neurotransmitters such as serotonin, dopamine, and GABA, which play crucial roles in mood regulation.
Exercise and Sleep
Exercise’s Beneficial Effects on Gut Health
Regular exercise has numerous benefits for gut health, including enhancing microbial diversity and reducing inflammation. It also positively impacts mental health, creating a holistic health approach.
The Role of Sleep in Maintaining the Gut-Brain Connection
Quality sleep is essential for maintaining a healthy gut-brain axis. Poor sleep can disrupt gut health and influence mental well-being, making sleep hygiene a critical aspect of overall health.
Stress, Mental Health Disorders and the Gut-Brain Axis
The Impact of Stress on Gut Health
Stress can significantly affect the gut, contributing to various gastrointestinal issues and altering gut microbiota composition. Chronic stress is particularly detrimental, leading to:
– Increased Gut Permeability: Stress can disrupt the gut barrier, allowing harmful substances to enter the bloodstream, which can trigger systemic inflammation.
– Altered Gut Motility: Stress can either speed up or slow down gut motility, leading to symptoms such as diarrhoea or constipation.
– Microbiota Imbalance: Chronic stress can reduce the diversity of the gut microbiota, promoting the growth of harmful bacteria over beneficial ones.
Mental health disorders, including depression, anxiety, and schizophrenia, have been linked to dysfunctions in the gut-brain axis. This connection is mediated through several mechanisms:
– Inflammation: Elevated levels of pro-inflammatory cytokines are often found in individuals with depression and anxiety, suggesting a role for systemic inflammation in these conditions.
– Neurotransmitter Imbalances: Dysbiosis can lead to altered production of neurotransmitters and their precursors, contributing to mood disorders.
– Hypothalamic-Pituitary-Adrenal (HPA) Axis Dysregulation: Chronic stress and dysbiosis can disrupt HPA axis function, leading to abnormal cortisol levels and contributing to mental health issues.
Mood and cognition.
Let us explore how inflammation influences them.
1. Bidirectional Communication: The gut and the brain communicate bidirectionally through various pathways, including the immune system. Inflammatory molecules released in the gut can travel through the bloodstream or stimulate the vagus nerve to reach the brain. Similarly, the brain can modulate immune responses in the gut. This bidirectional communication allows inflammation to impact both gut function and brain health.
2. Impact on Mood: Inflammation in the gut can disrupt the balance of neurotransmitters, such as serotonin and dopamine, which play crucial roles in regulating mood. Inflammatory molecules can interfere with the synthesis, release, and reuptake of these neurotransmitters, leading to imbalances that contribute to mood disturbances. Studies have linked increased levels of inflammation with an increased risk of developing mood disorders, such as depression and anxiety.
3. Cognitive Impairment: Inflammation can also impact cognitive function. Chronic inflammation in the gut can activate immune cells and release pro-inflammatory cytokines that can cross the blood-brain barrier and reach the brain. These cytokines can trigger neuroinflammation and impair normal brain function, leading to cognitive deficits. Inflammatory molecules can disrupt neural circuits involved in memory, attention, and executive function, potentially contributing to conditions like brain fog, cognitive decline, and even neurodegenerative disorders.
4. Neuroplasticity and Neurogenesis: Inflammation can disrupt neuroplasticity, which is the brain’s ability to adapt and change in response to experiences and stimuli. Chronic inflammation can interfere with synaptic plasticity and impair the formation of new neural connections. Additionally, inflammation can inhibit neurogenesis, the process of generating new neurons. Reduced neuroplasticity and neurogenesis can impact learning, memory, and overall cognitive function.
5. Microglial Activation: Microglia, the immune cells of the central nervous system, play a crucial role in the brain’s response to inflammation. When inflammation occurs, microglia can become activated and release pro-inflammatory molecules. While inflammation is an important defence mechanism, chronic microglial activation can lead to sustained neuroinflammation, contributing to long-term cognitive and mood disturbances.
It is important to note that the impact of inflammation on mood and cognition may vary among individuals. Some people may be more susceptible to the effects of inflammation due to genetic factors, previous exposure to stressors, or other underlying health conditions. Additionally, the gut microbiome and its composition can influence the degree of inflammation and its impact on the gut-brain axis.
The gut microbiome composition plays a crucial role in influencing the gut-brain axis and the risk of mood disorders. Here is how it influences the gut-brain axis and mood disorders:
- Neurotransmitter Production: The gut microbiome is involved in the production and regulation of neurotransmitters, such as serotonin, dopamine, and gamma-aminobutyric acid (GABA). These neurotransmitters play essential roles in regulating mood, emotions, and behaviour . Certain gut bacteria have the ability to produce and modulate these neurotransmitters, influencing the communication between the gut and the brain. An imbalance in the gut microbiome composition can disrupt neurotransmitter production and contribute to mood disorders.
- Immune System Modulation: The gut microbiome interacts closely with the immune system. A healthy and diverse gut microbiome helps maintain a balanced immune response. Imbalances or dysbiosis in the microbiome composition can lead to chronic low-grade inflammation and immune dysregulation. This chronic inflammation can trigger immune responses that can affect the gut-brain axis and increase the risk of mood disorders.
- Gut Barrier Function: The gut microbiome plays a role in maintaining the integrity and function of the gut barrier. The gut barrier acts as a protective barrier, preventing harmful substances from entering the bloodstream. Disruptions in the gut microbiome composition can compromise the gut barrier function, leading to increased permeability or “leaky gut.” This increased permeability allows the passage of toxins, bacteria, and inflammatory molecules into the bloodstream, potentially triggering systemic inflammation and affecting brain function.
- Metabolite Production: The gut microbiome produces various metabolites, including short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. These metabolites have been shown to have neuroprotective effects, reduce inflammation, and support brain health. SCFAs can influence the gut-brain axis by modulating immune responses, neurotransmitter production, and gene expression in the brain. Alterations in the gut microbiome composition can impact the production of these metabolites, potentially affecting the risk of mood disorders.
- Stress Response: The gut microbiome can also influence the stress response and the regulation of the hypothalamic-pituitary-adrenal (HPA) axis, which controls the release of stress hormones like cortisol. Certain gut bacteria can produce metabolites that can influence the HPA axis, either promoting or mitigating stress responses. Dysbiosis in the gut microbiome composition can disrupt this delicate balance and contribute to altered stress responses and mood disorders.
It is important to note that while the gut microbiome composition is associated with mood disorders, it does not necessarily cause them. Multiple factors, including genetics, environment, lifestyle, and individual susceptibility, contribute to the development of mood disorders. However, maintaining a healthy and diverse gut microbiome through a balanced diet, regular exercise, minimizing stress, and avoiding unnecessary antibiotics can support overall gut and brain health.
Research in the field of gut microbiome and mood disorders is ongoing, and further studies are needed to fully understand the complexities of this relationship. However, interventions aimed at modulating the gut microbiome, such as probiotics, prebiotics, and dietary changes, hold promise as potential strategies for improving mood and mental well-being.
Neurodegenerative Diseases and the Gut-Brain Axis
Parkinson’s disease (PD) is a neurodegenerative disorder characterised by the loss of dopamine-producing neurons in the brain. Recent research suggests that gut health may play a role in the development and progression of PD:
– Gut Microbiota Changes: Individuals with PD often exhibit altered gut microbiota composition, with a decrease in beneficial bacteria and an increase in harmful ones.
– Alpha-Synuclein: Misfolded alpha-synuclein proteins, a hallmark of PD, have been found in the gut before appearing in the brain, suggesting that the disease may originate in the gut.
The proposed mechanisms by which gut-derived metabolites exert neuroprotective effects are still being explored, but here are some of the potential mechanisms that have been suggested:
- Anti-inflammatory Effects: Many gut-derived metabolites, such as short-chain fatty acids (SCFAs) and indole derivatives, have been shown to possess anti-inflammatory properties. They can modulate immune cell function, reduce the production of pro-inflammatory molecules, and promote the release of anti-inflammatory molecules. By dampening inflammation in the brain, these metabolites may help protect neurons and mitigate the neuroinflammation associated with neurodegenerative diseases.
- Antioxidant Properties: Several gut-derived metabolites, including indole derivatives, have been reported to exhibit antioxidant effects. Oxidative stress, caused by an imbalance between the production of reactive oxygen species (ROS) and the body’s antioxidant defenses, is believed to contribute to neuronal damage in neurodegenerative disorders. The antioxidant properties of these metabolites may help counteract oxidative stress and protect neurons from damage.
- Modulation of Neurotransmitter Systems: Certain gut-derived metabolites, such as serotonin and gamma-aminobutyric acid (GABA), can act as neurotransmitters or modulate neurotransmitter systems in the brain. Neurotransmitters play a critical role in neuronal communication and function. By influencing neurotransmitter systems, these metabolites may help regulate neuronal activity, enhance neuroplasticity, and contribute to neuroprotective effects.
- Enhancement of Neurotrophic Factors: Neurotrophic factors are proteins that support the growth, survival, and maintenance of neurons. Some gut-derived metabolites, including SCFAs, have been shown to increase the expression of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), in the brain. Elevated levels of neurotrophic factors can promote neuronal health, stimulate neurogenesis (the formation of new neurons), and enhance synaptic plasticity.
- Modulation of the Gut-Brain Axis: The gut microbiome and its metabolites communicate with the brain through the gut-brain axis, involving neural, immune, and endocrine pathways. Gut-derived metabolites can influence the signaling along this axis, affecting neuroinflammatory responses, neurotransmitter production, and other processes relevant to neurodegenerative diseases. By modulating this communication, these metabolites may exert neuroprotective effects.
It is important to note that the specific mechanisms and effects of gut-derived metabolites may vary depending on the metabolite, the specific neurodegenerative disease being studied, and individual differences. Further research is needed to fully understand these mechanisms and their potential therapeutic applications.
Alzheimer’s Disease
Alzheimer’s disease (AD) is characterised by the accumulation of amyloid-beta plaques and tau tangles in the brain, leading to cognitive decline. The gut-brain axis may contribute to AD through:
– Inflammation: Chronic inflammation, driven by dysbiosis and gut permeability, is linked to AD pathology.
– Microbiota Composition: Changes in gut microbiota composition have been observed in AD patients, suggesting a role for gut health in disease progression.
The role of the gut microbiome in mental disorders and neurodegenerative disorders is an exciting area of research that has gained attention in recent years. While the exact mechanisms are still being explored, emerging evidence suggests that the gut microbiome can influence brain health and contribute to the pathogenesis of these conditions.
Potential Therapeutic Approaches
– Probiotics and Prebiotics: Probiotics are live microorganisms that can have beneficial effects on the gut microbiome, while prebiotics are substances that promote the growth of beneficial gut bacteria. These interventions aim to restore a healthy gut microbiome and have shown promise in preclinical and some clinical studies for mental disorders and neurodegenerative diseases.
– Dietary Interventions: Modifying the diet to promote a healthy gut microbiome has been explored as a potential therapeutic approach. A diet rich in fibre and plant-based foods can support the growth of beneficial gut bacteria and the production of metabolites with potential neuroprotective effects.
– Faecal Microbiota Transplantation (FMT): FMT involves transferring faecal material from a healthy donor to a recipient to restore a healthy gut microbiome. While still in the experimental stage, FMT has shown some promise in certain conditions, including recurrent Clostridioides difficile infection and some cases of Parkinson’s disease.
It is important to note that the field of gut microbiome research is still evolving, and the specific mechanisms and therapeutic applications are yet to be fully elucidated. Further research is needed to better understand the complex interactions between the gut microbiome, mental disorders, and neurodegenerative diseases.
– Alterations in Specific Taxa: Studies have reported alterations in the abundance of specific bacterial taxa in individuals with neurodegenerative diseases. For example, reductions in the abundance of butyrate-producing bacteria, such as those from the Roseburia and Faecalibacterium genera, have been observed in individuals with Alzheimer’s disease.
– Metabolites: The production of specific metabolites by the gut microbiome, such as urolithins and SCFAs, may have implications for neurodegenerative diseases. For instance, alterations in the production of urolithins have been associated with Parkinson’s disease.
There are several gut-derived metabolites that have shown promising neuroprotective potential in research. While the field is still evolving and more studies are needed, here are a few metabolites:
- Butyrate: Butyrate, a short-chain fatty acid (SCFA), has demonstrated notable neuroprotective properties in various studies. It has been shown to possess anti-inflammatory effects, improve mitochondrial function, promote neurogenesis, and enhance synaptic plasticity. These actions contribute to its potential neuroprotective effects in neurodegenerative diseases.
- Indole-3-Propionic Acid (IPA): IPA, an indole derivative produced by gut bacteria, has shown promise as a neuroprotective metabolite. It displays antioxidant and anti-inflammatory properties and has been observed to protect neurons against oxidative stress, reduce neuroinflammation, and enhance cognitive function in animal models of neurodegenerative diseases.
- Urolithins: Urolithins are metabolites derived from ellagitannins, which are compounds found in certain fruits and nuts. These metabolites are produced by gut bacteria and have shown neuroprotective effects. Urolithins have been found to enhance mitochondrial function, stimulate neurogenesis, and exhibit anti-inflammatory properties, potentially contributing to their neuroprotective potential.
- Tryptamine: Tryptamine is a neuroactive metabolite derived from the amino acid tryptophan. It has been shown to possess antioxidant and anti-inflammatory properties, potentially contributing to its neuroprotective effects. Tryptamine has demonstrated the ability to protect neurons against oxidative stress and reduce neuroinflammation in various experimental models.
Specific gut bacteria species can influence the production of neurotransmitters like serotonin and impact mental health. Here are some examples:
1. Lactobacillus and Bifidobacterium: Certain species of Lactobacillus and Bifidobacterium have been found to play a role in the production and regulation of serotonin. These bacteria can produce tryptophan, an amino acid precursor of serotonin. By increasing the availability of tryptophan, Lactobacillus and Bifidobacterium can potentially enhance serotonin synthesis in the gut. Serotonin, often referred to as the “happy neurotransmitter,” is involved in regulating mood, emotions, and sleep. Imbalances in serotonin have been linked to mood disorders such as depression and anxiety.
2. Escherichia coli: Some strains of Escherichia coli can also influence serotonin production. These strains can produce enzymes that convert tryptophan into a compound called 5-hydroxytryptophan (5-HTP), which is an intermediate step in serotonin synthesis. By increasing 5-HTP levels they enhance serotonin production.
3. Prevotella and Coprococcus: Certain species within the Prevotella and Coprococcus genera have been associated with higher levels of tryptophan metabolism. These bacteria can break down tryptophan into various metabolites, including indole-3-propionic acid (IPA). IPA has been shown to have neuroprotective effects and may influence serotonin levels and brain health.
4. Akkermansia muciniphila: Akkermansia muciniphila is a gut bacterium that has gained attention for its potential impact on mental health. While its direct influence on serotonin production is not fully understood, studies have shown that Akkermansia muciniphila can promote gut barrier integrity, reduce inflammation, and modulate metabolism. These effects may indirectly influence serotonin levels and mental health.
It is important to note that the relationship between specific gut bacteria species and neurotransmitter production is still being explored, and research in this field is ongoing. The gut microbiome is a complex ecosystem with numerous bacterial species, and their interactions can be intricate. The presence or absence of specific bacteria alone may not be the sole determinant of neurotransmitter production or mental health outcomes. The overall composition and balance of the gut microbiome, as well as interactions between different bacterial species, may collectively influence neurotransmitter levels and mental well-being.
However, these findings highlight the potential importance of maintaining a diverse and balanced gut microbiome through a healthy diet, regular exercise, stress management, and other lifestyle factors. Such practices can support the growth of beneficial bacteria and promote overall gut and mental health.
Conclusion
The gut-brain axis represents a fascinating and complex system of bidirectional communication that plays a crucial role in maintaining overall health. Emerging research highlights the significant impact of gut health on mental health, stress response, and neurodegenerative diseases. By understanding and leveraging this connection, we can develop novel therapeutic strategies to improve both gut and brain health.
As we continue to unravel the mysteries of this intricate system, the future holds exciting possibilities for enhancing well-being and preventing disease through a deeper understanding of the gut-brain connection. Whether through diet, probiotics, stress management, or innovative therapies, nurturing the gut-brain axis offers a holistic path to better health and improved quality of life.
How Can I Improve My Gut-Brain Health?
+ Maintain a balanced diet rich in fibre, fruits, and vegetables.
+ Incorporate probiotics and prebiotics.
+ Engage in regular exercise and ensure quality sleep.
+ Practice stress management techniques like mindfulness and meditation.
Are There Specific Foods to Avoid for Better Gut-Brain Health?
+ Avoid processed foods high in sugar and unhealthy fats.
+ Limit consumption of artificial additives and preservatives.
+ Reduce intake of alcohol and caffeine.
What Are the Symptoms Indicating a Problem with the Gut-Brain Axis?
+ Digestive issues like bloating, pain, and irregular bowel movements.
+ Mood disorders such as depression and anxiety.
+ Chronic fatigue and cognitive difficulties.
+ Unexplained weight changes and immune system dysfunctions.
This article is not intended to replace professional medical advice. If you have specific health concerns or conditions, consult with a healthcare professional for personalised guidance.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered as medical advice. Always consult with a healthcare professional before making any changes to your diet or lifestyle.