Part 3 of the 3 part article titled. The Microbiome’s Influence on Breast Cancer Immunity: Unveiling the Gut-Breast Connection
Table of Contents
Dietary interventions to support beneficial bacteria
One of the most effective ways to support a healthy microbiome is through dietary interventions. By making strategic choices in your diet, you can cultivate beneficial bacteria that may help reduce your risk of breast cancer.
Fibre-rich foods
Increasing your intake of fibre-rich foods is crucial for maintaining a diverse and healthy gut microbiome. Fibre acts as a prebiotic, providing nourishment for beneficial bacteria. Here are some excellent sources of dietary fibre:
- Whole grains (e.g., quinoa, brown rice, oats)
- Legumes (e.g., lentils, chickpeas, black beans)
- Fruits (e.g., berries, apples, pears)
- Vegetables (e.g., broccoli, brussel sprouts, sweet potatoes)
- Nuts and seeds (e.g., almonds, chia seeds, flaxseeds)
Aim to incorporate a variety of these foods into your daily diet to support a diverse microbiome. The American Heart Association recommends consuming 25-30 grams of fibre per day for adults.
Fermented foods
Fermented foods are rich in probiotics, which are live beneficial bacteria that can contribute to a healthy gut microbiome. Including fermented foods in your diet can help introduce and maintain beneficial bacteria in your gut. Some popular fermented foods include:
- Yogurt (look for varieties with live active cultures)
- Kefir
- Kombucha
- Sauerkraut
- Kimchi
- Miso
- Tempeh
Try to incorporate at least one serving of fermented foods into your daily diet to support your gut microbiome.
Polyphenol-rich foods
Polyphenols are plant compounds that have been shown to have anti-inflammatory and antioxidant properties. They can also act as prebiotics, supporting the growth of beneficial bacteria in your gut. Some excellent sources of polyphenols include:
- Berries (e.g., blueberries, strawberries, raspberries)
- Dark chocolate (70% cocoa or higher)
- Green tea
- Red wine (in moderation)
- Olive oil
- Herbs and spices (e.g., turmeric, oregano, rosemary)
Incorporating these foods into your diet can help support a healthy microbiome and potentially reduce your risk of breast cancer.
Foods to limit or avoid
Just as there are foods that can support a healthy microbiome, there are also foods that can negatively impact your gut bacteria. To maintain optimal gut health and potentially reduce your breast cancer risk, consider limiting or avoiding:
- Processed foods high in artificial additives and preservatives
- Refined sugars and high-fructose corn syrup
- Excessive red meat consumption
- Alcohol (excessive consumption)
- Artificial sweeteners
By reducing your intake of these foods, you can help create an environment in your gut that supports beneficial bacteria and potentially reduces breast cancer risk.
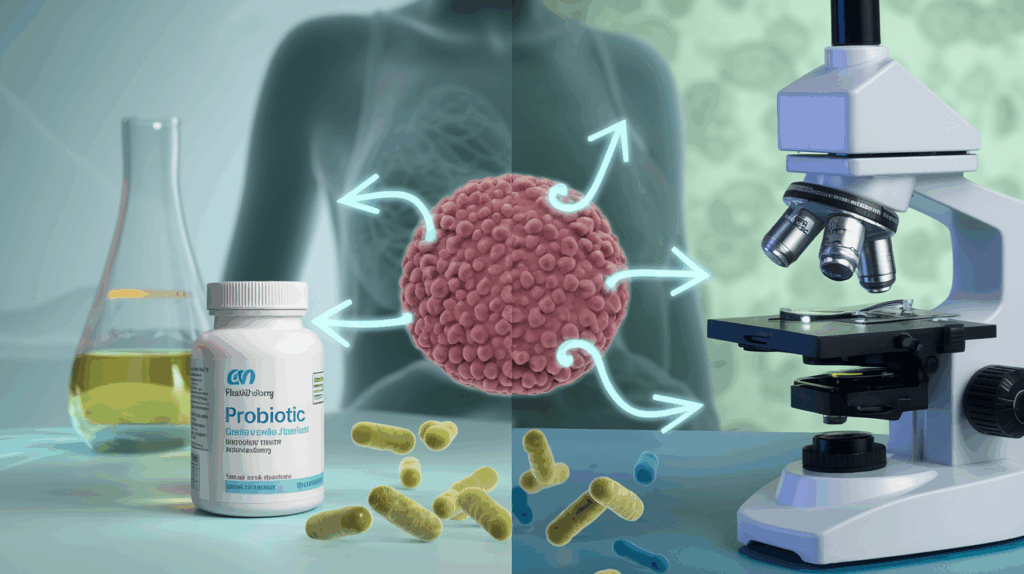
Probiotic and prebiotic supplementation
While dietary interventions are crucial for supporting a healthy microbiome, supplementation with probiotics and prebiotics can provide additional support.
Probiotics
Probiotics are live microorganisms that, when consumed in adequate amounts, can provide health benefits. While more research is needed to fully understand their role in breast cancer prevention, some studies have shown promising results
- Types of probiotics: Common probiotic strains include Lactobacillus, Bifidobacterium, and Saccharomyces boulardii.
- Dosage: The optimal dosage can vary depending on the specific strain and your individual needs. Consult with a healthcare professional for personalised recommendations.
- Timing: Take probiotics on an empty stomach or 30 minutes before a meal for best absorption.
- Quality matters: Choose high-quality supplements from reputable manufacturers to ensure potency and effectiveness.
| Probiotic Strain | Potential Benefits |
| Lactobacillus acidophilus | May help reduce inflammation and support immune function |
| Bifidobacterium longum | May help improve gut barrier function and reduce oxidative stress |
| Lactobacillus rhamnosus | May help modulate immune responses and reduce inflammation |
Remember that while probiotics can be beneficial, they are not a substitute for a healthy diet and lifestyle. Always consult with your healthcare provider before starting any new supplement regimen.
Prebiotics
Prebiotics are non-digestible fibres that serve as food for beneficial bacteria in your gut. Some common prebiotic supplements include:
- Inulin
- Fructooligosaccharides (FOS)
- Galactooligosaccharides (GOS)
- Resistant starch
When choosing a prebiotic supplement, look for products that contain a mix of different prebiotic fibres to support a diverse range of beneficial bacteria. Start with a low dose and gradually increase to avoid digestive discomfort.
Lifestyle changes for optimal gut health
In addition to dietary interventions and supplementation, certain lifestyle changes can significantly impact your gut microbiome and potentially reduce your risk of breast cancer. Here are some key areas to focus on:
Stress management
Chronic stress can negatively impact your gut microbiome, potentially increasing inflammation and weakening your immune system. To support optimal gut health and potentially reduce breast cancer risk, consider incorporating stress-reduction techniques into your daily routine:
- Meditation or mindfulness practices
- Deep breathing exercises
- Yoga or tai chi
- Regular exercise
- Spending time in nature
- Engaging in hobbies or creative activities
Find stress-management techniques that work best for you and make them a regular part of your routine.
Regular exercise
Physical activity not only helps reduce stress but also directly impacts your gut microbiome. Regular exercise has been shown to increase the diversity of gut bacteria and promote the growth of beneficial species. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, as recommended by the World Health Organization.
Adequate sleep
Poor sleep quality and insufficient sleep duration can negatively impact your gut microbiome. To support optimal gut health:
- Aim for 7-9 hours of sleep per night
- Establish a consistent sleep schedule
- Create a relaxing bedtime routine
- Avoid screens for at least an hour before bed
- Keep your bedroom cool, dark, and quiet
Avoiding unnecessary antibiotics
While antibiotics are sometimes necessary, overuse can disrupt your gut microbiome. To protect your beneficial bacteria:
- Only take antibiotics when prescribed by a healthcare professional
- Complete the full course of antibiotics as directed
- Consider taking probiotics during and after antibiotic treatment to help restore beneficial bacteria
By implementing these lifestyle changes alongside dietary interventions and appropriate supplementation, you can create an environment that supports a healthy gut microbiome. This, in turn, may help strengthen your immune system and potentially reduce your risk of breast cancer. Remember that maintaining a healthy microbiome is an ongoing process, so consistency is key in reaping the potential benefits for breast cancer prevention.
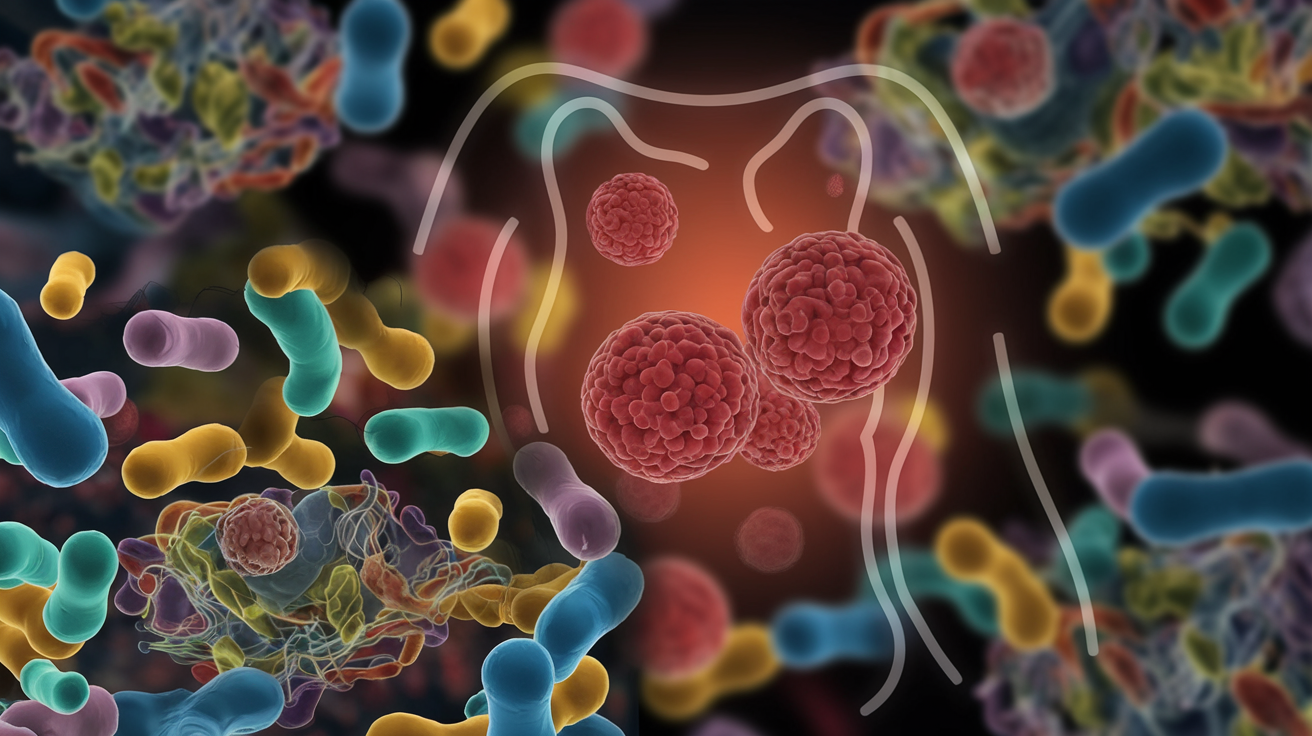
Microbiome-Based Approaches in Breast Cancer Treatment
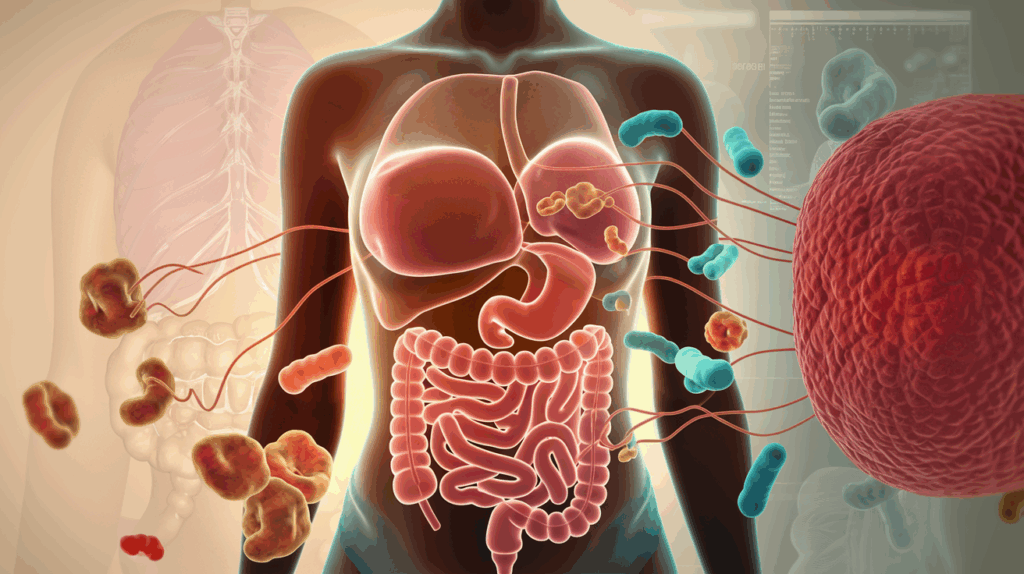
Enhancing immunotherapy efficacy
As we look into microbiome-based approaches in breast cancer treatment, it is good to understand how the gut microbiome can enhance the efficacy of immunotherapy. Immunotherapy has revolutionised cancer treatment, but its effectiveness varies among patients. Recent research suggests that the gut microbiome plays a role in determining the success of these treatments.
The gut microbiome can influence immunotherapy efficacy in several ways:
- Modulation of immune responses
- Regulation of checkpoint inhibitors
- Production of metabolites that affect cancer cells
- Enhancement of T-cell function
Let us explore these mechanisms in more detail:
Modulation of immune responses
The gut microbiome interacts closely with the immune system, shaping its responses to various stimuli, including cancer cells. Certain beneficial bacteria can stimulate the production of pro-inflammatory cytokines and activate immune cells, creating a more favourable environment for immunotherapy to work effectively.
For instance, studies have shown that patients with a diverse gut microbiome, particularly those with an abundance of Bifidobacterium species, respond better to immune checkpoint inhibitors. These bacteria help activate dendritic cells, which in turn stimulate T-cells to recognise and attack cancer cells more efficiently.
Regulation of checkpoint inhibitors
Checkpoint inhibitors, such as PD-1 and CTLA-4 inhibitors, have shown remarkable success in treating various cancers, including breast cancer. The gut microbiome can influence the expression of these checkpoint molecules, affecting the overall efficacy of the treatment.
| Microbiome Composition | Effect on Checkpoint Inhibitors |
| High Akkermansia muciniphila | Improved response to PD-1 inhibitors |
| Abundant Faecalibacterium | Enhanced efficacy of CTLA-4 inhibitors |
| Low diversity | Reduced response to checkpoint inhibitors |
Production of metabolites affecting cancer cells
The gut microbiome produces a wide range of metabolites that can directly or indirectly affect cancer cells. For example:
- Short-chain fatty acids (SCFAs): Produced by bacteria like Faecalibacterium prausnitzii, SCFAs can inhibit histone deacetylases, leading to epigenetic changes that may enhance the effectiveness of immunotherapy.
- Secondary bile acids: Certain gut bacteria can convert primary bile acids into secondary bile acids, which have been shown to modulate anti-tumor immune responses.
Enhancement of T-cell function
T-cells are crucial players in the immune response against cancer. The gut microbiome can enhance T-cell function in several ways:
- Promoting T-cell differentiation
- Enhancing T-cell infiltration into tumours
- Increasing T-cell memory formation
By optimising the gut microbiome, we can potentially boost these T-cell functions, making immunotherapy more effective in treating breast cancer.
Reducing treatment side effects
While immunotherapy and other cancer treatments can be highly effective, they often come with significant side effects that can impact a patient’s quality of life. Interestingly, the gut microbiome may play a role in mitigating these side effects, offering a promising avenue for improving treatment outcomes.
Alleviating gastrointestinal side effects
Many cancer treatments, including chemotherapy and radiation therapy, can cause severe gastrointestinal (GI) side effects such as nausea, diarrhea, and inflammation. The gut microbiome can help reduce these side effects in several ways:
- Maintaining gut barrier integrity
- Producing anti-inflammatory compounds
- Metabolising drugs to reduce toxicity
For example, probiotics containing Lactobacillus and Bifidobacterium species have shown promise in reducing chemotherapy-induced diarrhea and mucositis.
Mitigating immune-related adverse events
Immune checkpoint inhibitors can sometimes lead to immune-related adverse events (irAEs) affecting various organs. Recent studies suggest that the gut microbiome composition may influence the likelihood and severity of these side effects.
| Microbiome Characteristic | Effect on irAEs |
| High diversity | Lower risk of severe irAEs |
| Abundance of Bacteroidetes | Reduced incidence of colitis |
| Presence of Faecalibacterium | Lower risk of immune-mediated diarrhea |
By modulating the gut microbiome, it may be possible to reduce the occurrence and severity of these side effects, allowing patients to continue their treatment regimens with fewer interruptions.
Reducing fatigue and improving overall well-being
Cancer-related fatigue is a common and debilitating side effect of many treatments. Emerging evidence suggests that the gut microbiome may play a role in modulating energy metabolism and inflammation, potentially affecting fatigue levels.
Strategies to optimise the gut microbiome, such as dietary interventions and probiotic supplementation, may help reduce fatigue and improve overall well-being during cancer treatment.
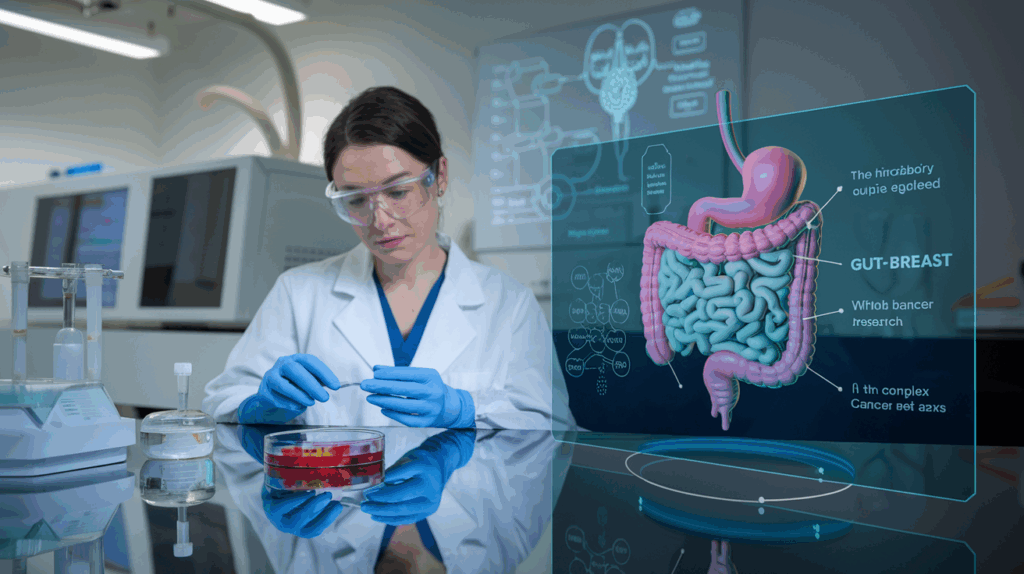
Personalised microbiome interventions
As our understanding of the gut-breast connection deepens, the potential for personalised microbiome interventions in breast cancer treatment becomes increasingly apparent. These tailored approaches take into account an individual’s unique microbiome composition and cancer characteristics to optimise treatment outcomes.
Microbiome profiling for treatment selection
By analysing a patient’s gut microbiome composition, clinicians may be able to predict which treatments are likely to be most effective and which may cause severe side effects. This information can guide treatment decisions, potentially improving outcomes and reducing unnecessary side effects.
For example:
- Patients with high levels of Akkermansia muciniphila may be more likely to respond well to PD-1 inhibitors.
- Those with a diverse microbiome rich in Faecalibacterium may have a better chance of success with CTLA-4 inhibitors.
Targeted probiotic interventions
Based on an individual’s microbiome profile and cancer characteristics, targeted probiotic interventions can be designed to:
- Enhance beneficial bacteria populations
- Reduce harmful bacteria
- Optimise the overall microbiome composition for better treatment outcomes
These interventions may involve specific probiotic strains, prebiotic supplements, or a combination of both, tailored to each patient’s needs.
Dietary modifications
Personalised dietary recommendations can help shape the gut microbiome to support cancer treatment. These may include:
- Increasing fibre intake to promote the growth of beneficial bacteria
- Incorporating fermented foods to introduce diverse probiotic strains
- Limiting processed foods and added sugars that may promote inflammation
By tailoring these dietary interventions to an individual’s microbiome profile and cancer treatment plan, clinicians can potentially enhance treatment efficacy and reduce side effects.
Future directions in microbiome-targeted therapies
The field of microbiome-based approaches in breast cancer treatment is rapidly evolving, with exciting developments on the horizon. As research continues to uncover the intricate relationships between the gut microbiome and breast cancer, several promising avenues for future therapies are emerging.
Engineered probiotics for targeted cancer therapy
Scientists are exploring the potential of genetically engineered probiotics that can:
- Deliver cancer-fighting compounds directly to tumour sites
- Enhance the immune system’s ability to recognise and attack cancer cells
- Modulate the tumour microenvironment to inhibit cancer growth
These “smart” probiotics could offer a more targeted and less toxic approach to cancer treatment, potentially working in synergy with existing therapies.
Microbiome-based biomarkers for treatment response
The gut microbiome may serve as a valuable source of biomarkers to predict treatment response and monitor disease progression. Researchers are working on developing:
- Microbial signatures that indicate likelihood of response to specific treatments
- Microbiome-based tests to detect early signs of treatment resistance or disease recurrence
These biomarkers could help clinicians make more informed decisions about treatment strategies and adjust therapies as needed.
Faecal microbiota transplantation (FMT) in cancer treatment
While still in its early stages, FMT shows promise as a potential adjunct therapy in cancer treatment. By transferring the gut microbiome from healthy donors or responsive patients, FMT could:
- Enhance the efficacy of immunotherapy
- Reduce treatment-related side effects
- Improve overall treatment outcomes
However, more research is needed to fully understand the safety and efficacy of FMT in cancer treatment.
Integration of microbiome data with other -omics approaches
The future of microbiome-targeted therapies lies in integrating microbiome data with other -omics approaches, such as genomics, proteomics, and metabolomics. This multi-omics approach will provide a more comprehensive understanding of the complex interactions between the gut microbiome, the host, and cancer.
| -Omics Approach | Contribution to Microbiome-Targeted Therapies |
| Genomics | Identify host genetic factors influencing microbiome composition |
| Proteomics | Understand microbiome-host protein interactions |
| Metabolomics | Analyse microbial metabolites affecting cancer progression |
| Transcriptomics | Study gene expression changes in response to microbiome modulation |
By combining these approaches, researchers can develop more sophisticated and effective microbiome-based strategies for breast cancer treatment.
Conclusion
As we look to the future, it is clear that microbiome-based approaches hold tremendous potential in revolutionising breast cancer treatment. From enhancing immunotherapy efficacy to reducing side effects and developing personalised interventions, the gut-breast connection offers exciting possibilities for improving patient outcomes and quality of life. With ongoing research and technological advancements, we can expect to see more innovative microbiome-targeted therapies emerging in the coming years, bringing us closer to more effective and personalised breast cancer treatments.
The intricate relationship between the microbiome and breast cancer immunity reveals a fascinating frontier in cancer research. By understanding the gut-breast connection, you can take proactive steps to support your overall health and potentially reduce your risk of breast cancer. From maintaining a balanced gut microbiome through diet and lifestyle choices to exploring innovative microbiome-based treatments, there are numerous ways to harness the power of these tiny organisms for your benefit.
As research in this field continues to evolve, stay informed about the latest developments and consult with healthcare professionals to incorporate microbiome-friendly strategies into your wellness routine. Remember, your microbiome is a powerful ally in the fight against breast cancer, and nurturing it can contribute to a stronger immune system and better overall health.
References
1.Front. Oncol. , 07 November 2022;Volume 12 – 2022 | https://doi.org/10.3389/fonc.2022.1037831
2.Kovács, T., Mikó, E., Vida, A. et al. Cadaverine, a metabolite of the microbiome, reduces breast cancer aggressiveness through trace amino acid receptors. Sci Rep 9, 1300 (2019). https://doi.org/10.1038/s41598-018-37664-7
3. Cells. 2019 Mar 29;8(4):293. doi: 10.3390/cells804029.
4. Microorganisms. 2022 Oct 17;10(10):2048. doi: 10.3390/microorganisms10102048
5. Cancers 2023, 15(2), 443; https://doi.org/10.3390/cancers15020443
6. EMBO Mol Med(2025)17: 219 – 234 https://doi.org/10.1038/s44321-024-00185-0
7. PROTEIN STRUCTURE AND FOLDINGVolume 294, Issue 49P18586-18599December 2019
8. Front. Microbiol. , 30 October 2023 Sec. Microorganisms in Vertebrate Digestive Systems.Volume 14 – 2023 | https://doi.org/10.3389/fmicb.2023.1272275
9. https://doi.org/10.1177/15347354241269870
This article is not intended to replace professional medical advice. If you have specific health concerns or conditions, consult with a healthcare professional for personalised guidance.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered as medical advice. Always consult with a healthcare professional before making any changes to your diet or lifestyle.